Ramadan is a month of spirituality and excitement for many Muslims around the world. However, for Muslims with diabetes, Ramadan can also present new challenges for managing diabetes while practising one’s faith.
From a religious perspective, Muslims who are ill, including Muslims managing chronic conditions such as diabetes, may be exempted from fasting. Allah ﷻ says in the Quran:
O you who have believed, decreed upon you is fasting as it was decreed upon those before you that you may become righteous – [Fasting for] a limited number of days. So whoever among you is ill or on a journey [during them] – then an equal number of days [are to be made up]. And upon those who are able [to fast, but with hardship] – a ransom [as substitute] of feeding a poor person [each day]. And whoever volunteers excess – it is better for him. But to fast is best for you, if you only knew.” (Quran, Surah Baqarah: 183-184)
For Muslims with diabetes and chronic illness on daily medications, it is highly recommended to consult one’s physician to determine whether patients with diabetes are able to fast in Ramadan.
Researchers find that “many patients with diabetes tend to ignore advice from specialists and insist on fasting during the month of Ramadan, which can result in potentially harmful consequences.” (1) A large multinational study (The Epidemiology of Diabetes and Ramadan (EPIDIAR) study) of 13 countries showed that in a clinic-based sample of Muslim patients with diabetes, 43% with type 1 diabetes and 79% with type 2 diabetes fasted for at least 15 days during the month of Ramadan. (2)
It is important to note that every patient has a unique medical history. Fasting in Ramadan is a serious decision that every patient needs to make in consultation with their doctors as to what adjustments need to be made for Ramadan, provided one is healthy enough to fast.
This article aims to empower Muslims with diabetes to dialogue with their doctor to make informed decisions as to whether or not to fast in Ramadan and to provide practical tips how to better manage your diabetes in Ramadan while fasting.
“Can I Fast in Ramadan with Diabetes?” Guidelines for Fasting In Patients with Diabetes
Your ability to fast in Ramadan is highly individual and depends upon many factors:
- The type of diabetes you have been diagnosed with (type 1 versus type 2 diabetes)
- Your medical history (the particulars of your diagnosis and any other medical conditions that increase your risk)
- Your history of diabetes management (eg. through lifestyle interventions, exercise and healthy eating)
- Your willingness & ability to proactively manage your diabetes in Ramadan (eg. self-monitoring of glucose levels, managing complications, maintaining a healthy food diet during Ramadan, exercise.)
Type 1 versus Type 2 Diabetes in Ramadan

Patients with type 1 versus type 2 diabetes may experience different challenges in determining if they are able to fast.
Type 2 diabetes: A patient’s ability to fast depends greatly on their management, lifestyle, and medical history. In the most optimistic case for a well-managed patient with a normal BMI who maintains a healthy lifestyle and relies on medical counsel, “Ramadan fasting would be acceptable for patients with well-balanced type 2 diabetes who are conscious of their disease and compliant with their diet and drug intake.” (7)
Patients with type 2 diabetes are most at-risk for hypoglycaemia. Each patient must individually consult with their doctor to inquire whether medication adjustment is possible to allow them to fast. See the next sections in this article for guidelines on what to ask your doctor to determine if you are able to fast, and how to safely manage your diabetes while fasting.
Type 1 diabetes: Managing type 1 diabetes in Ramadan poses greater risks:
- Due to the high risk of hypoglycemia, hyperglycemia, and diabetic ketoacidosis, individuals with Type 1 diabetes may find fasting challenging, especially those with poor diabetes control and comorbidities. (6)
Patients with well-managed type 1 diabetes may still consult with their doctor to inquire as to their fasting capabilities. See the next sections in this article for guidelines on what to ask your doctor to determine if you are able to fast, and how to safely manage your diabetes while fasting.
All patients with type 1 and type 2 diabetes are encouraged to assess their level of risk with their doctor before deciding to fast in Ramadan:
Risks of Fasting in Ramadan with Diabetes
Numerous studies have shown that the majority of Muslim patients with diabetes are passionate about the fasting in Ramadan. Unfortunately, most are unaware (or willfully ignore) many possible risks and complications of fasting, which include hyperglycaemia, hypoglycaemia, and increased risk of dehydration and thrombosis (3) .
Fasting during the day influences the control of diabetes because of changes in meal times, the type of food eaten and daily lifestyle. Therefore, there is high risk of developing acute complications like hypoglycemia or ketoacidosis during fasting. The major risk of diabetics who fast during Ramadan is hypoglycemia. On the other hand, the excessive consumption of sweet and fried foods especially with the Iftar meal may pre-dispose to hyperglycemia. (4)
In order to avoid these negative health consequences, it is important to understand what these terms mean for you and your diagnosis.
Risk #1 – Hypoglycaemia
A patient’s blood glucose level drops too low below 4mmol/L or 70 mg/dL. This is especially a risk during Ramadan for patients on insulin or other glucose-lowering diabetes medications. Any medication that lowers your blood glucose has the potential to induce a hypoglycaemic state during fasting.
From the American Diabetes Association:
- Each person’s reaction to hypoglycemia is different, so it’s important that you learn your own signs and symptoms when your blood glucose is low.
- The only sure way to know whether you are experiencing hypoglycemia is to check your blood glucose, if possible. If you are experiencing symptoms and you are unable to check your blood glucose for any reason, treat the hypoglycemia. Severe hypoglycemia has the potential to cause accidents, injuries, coma, and death.
Risk #2 – Hyperglycaemia
A patient’s blood glucose level becomes elevated (7.0 mmol/L or 126 mg/dL). This is a particular concern after excessive consumption of sweet and fried foods especially with the Iftar meal. Note that hyperglycaemia may be asymptomatic and harder to detect.
From the American Diabetes Association:
- Hyperglycemia is the technical term for high blood glucose (blood sugar). High blood glucose happens when the body has too little insulin or when the body can’t use insulin properly.
Risk #3 – Dehydration
Dehydration is a particular concern for Muslims with diabetes during long fasting hours, and even more so in hot summer climates. Dehydration during Ramadan fasting may affect or worsen kidney function. Dehydration is dangerous as it may also lead to Ketoacidosis.
From the Hamad Medical Corporation:
- Dehydration can result in a higher blood viscosity (stickiness), which increases the chances of thrombosis (blood clots). For diabetics who choose to fast during Ramadan, it is important to drink plenty of water during non-fasting hours. Staying hydrated can help prevent dehydration and associated complications.
Risk #4 – Ketoacidosis
Ketoacidosis: Life-threatening state associated with poorly managed hyperglycemia (see above).
From the American Diabetes Association:
- If you fail to treat hyperglycemia, a condition called ketoacidosis (diabetic coma) could occur. Ketoacidosis develops when your body doesn’t have enough insulin. Without insulin, your body can’t use glucose for fuel, so your body breaks down fats to use for energy.
- When your body breaks down fats, waste products called ketones are produced. Your body cannot tolerate large amounts of ketones and will try to get rid of them through the urine. Unfortunately, the body cannot release all the ketones and they build up in your blood, which can lead to ketoacidosis.
- Ketoacidosis is life-threatening and needs immediate treatment. Talk to your doctor about how to handle this condition.
Muslim patients with diabetes who choose to fast put their health in danger if making the decision to fast without consultation with their doctor and medical approval. Some patients are NOT able to fast given their medical history. Even if a patient IS healthy enough to fast, they need to adjust their medication based on medical recommendations, be aware of risks and complications and ensure proper lifestyle strategies are in place to successfully fast safely.
Current research guidelines categorise patients with diabetes based on their level of risk when fasting in Ramadan. Low-risk patients may be more likely to be able to fast safely, whereas high-risk patients may be advised to abstain from fasting.
Table 1. Risk Stratification in Patients With Diabetes Who Fast During RamadanNote. Reprinted [adapted] from “Management of people with diabetes wanting to fast during Ramadan,” by E. Hui et al. Hui et al., 2010, BMJ, 340, 1407. Copyright 2017 by “BMJ”.
How to Speak With Your Doctor To Determine If you Can Fast
In order to determine your ability to fast, use the following guidelines to engage in a productive dialogue with your doctor:
- Share with your doctor what Ramadan fasting entails: If your doctor is not aware of Ramadan, avoid feeling misunderstood or unsupported by sharing with your doctor your desire to fast in Ramadan, and the conditions in which you will be fasting.
-
- Tell your doctor how many hours you will be fasting from Suhoor to Iftar – remember there is a BIG difference between a 10-hour fast versus an 18-hour fast for a patient with diabetes!
- Inform your doctor that you cannot eat OR drink during this time,
-
- Share with your doctor new research guidelines pertaining to diabetes management in Ramadan: Print out and bring the following Peer-Reviewed Article in the Journal of Family Medicine and Primary Care on physician treatment and management guidelines for patients with diabetes to your appointment, or send to your doctor before-hand. This article will help your physician use the latest medical guidelines to inform your diabetes management during Ramadan.
- Understand the medication you are on: Your medication has a big impact on your ability to fast in Ramadan. Ask your doctor questions to help you understand your treatment options in Ramadan:
-
- Can your medication cause your blood sugar to go very low? In which case your doctor may reduce your medication dosage during Ramadan.
- Ask your doctor: “If I decrease the amount of Insulin I am taking, will I be able to fast?” This question will elicit a good conversation to assess the potential risk of fasting for your diagnosis – also an effective exercise plan can naturally reduce your need for insulin medication
-
- Ask what lifestyle interventions, such as healthy eating and exercise you can engage in to have a more successful Ramadan:
-
- Your doctor may refer you to a dietitian to help you ensure your food intake in Ramadan is healthy and safe for a patient with diabetes
- Exercise can improve insulin sensitivity and improve your prognosis for fasting in Ramadan. Speak to your doctor about how you can improve your condition using physical exercise and make it a goal to improve your health by next Ramadan to be able to fast in a safe, healthy way!
- Kidney function can be improved in overweight patients after weight loss. Safe weight loss may allow a patient to fast safely in future Ramadans!
- Ensure your family is aware of your unique needs as a patient with diabetes. If your family is on board with preparing and eating diabetic-friendly, low carb meals, you are much more likely to avoid complications while fasting.
-
- Ask your doctor about monitoring & managing complications:
-
- Self-monitoring of blood glucose levels is essential in safe management of diabetes in Ramadan. Discuss with your doctor how often you should be checking your blood sugar.
-
Self-monitoring of blood glucose (SMBG) in Ramadan is an important tool during Ramadan for people with diabetes to provide the information about glucose variability, which can lead to detection and prevention of hypoglycaemia as well as hyperglycaemia. This can also certainly help in behaviour change of diet and physical activities during Ramadan. The frequency of monitoring would depend on the type of treatment, the glycaemic control and the lifestyle of the individual. It is also recommended for all people with diabetes to help detect postprandial hyperglycaemia, which is not unusual in many people with diabetes during Ramadan. (5)
-
-
- Involve & Educate your family in being able to recognise symptoms of hypoglycaemia, hyperglycaemia and dehydration. A patient’s family should recognise these symptoms as the patient’s judgement may not be sound during hypoglycaemic incident. Bring your spouse to your medical appointment to ensure you have family support during Ramadan. If symptoms arise, you and your family must be prepared to help you break your fast immediately.
-
4 Steps to Managing Your Diabetes in Ramadan
Once you have consulted with your doctor and have been medically cleared to fast, it is you and your family’s responsibility to ensure your health and safety by effective management of your diabetes during your fast.
Table 2. 4 Steps For Safe Fasting For Patients With Diabetes Note. Reprinted [adapted] from “Ramadan focused diabetes education; a much needed approach,” by M. Hassanein. Hassanein, 2015, Journal of Pakistan Medical Association, 65, 77. Copyright 2015 by “Journal of Pakistan Medical Association”.
Dietary Food Choices Make a BIG Difference: Adjusting Your Ramadan Diet For Safe Diabetes Management While Fasting
Your food choices at Suhoor and Iftar have a profound impact on the management of your diabetes. If you are serious in your desire to fast in Ramadan, you must be responsible in ensuring your food choices are healthy in Ramadan. Download our FREE Ramadan healthy eating checklist to help you eat the healthy, fuelling foods you need to experience your healthiest Ramadan, ever inshAllah!
Additionally, adhere to the following nutrition guidelines specifically for Muslim patients with diabetes from Registered Dietitian Noura Sheikhalzoor:
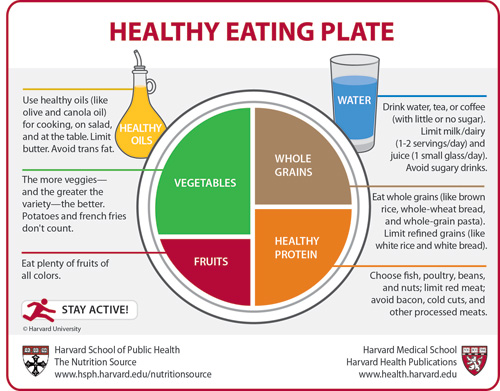
- PORTION CONTROL: Be wary of large portions of carbohydrates, including rice, potatoes, bread, naan, etc. At your meals, ensure that you do not exceed 1 handful of carbohydrates. You may find the following Harvard Healthy Plate diagram helpful to help control your carbohydrates:
- Hydrate aggressively during non-fasting intervals: Keep a water bottle with you during Taraweh and aim to drink 10 glasses of water.
- Smaller, spread out meals: Instead of eating 2 huge meals at suhoor and iftar, try to split your iftar meal into 2 smaller meals. Aim to eat 3 smaller meals during non-fasting intervals, instead of 2 huge meals.
- Be wary of simple refined sugars like sugar in desserts and white bread or rice. Simple sugars are particularly concerning for patients with diabetes because these simple carbohydrates spike your blood sugar immediately after eating. For patients with diabetes, your blood sugar may drop below the normal range after eating simple sugars. For patients with diabetes, try using stevia as a diabetic-friendly sugar replacement in desserts, tea or coffee. Avoid sugar-sweetened beverages and choose water, milk or stevia-sweetened tea instead.
- Swap simple carbohydrates for complex carbohydrates higher in fibre including wholegrains, legumes (chickpeas, beans), nuts, vegetables and fruits. These carbohydrates will raise your blood sugar slower and more controlled.
- Balance carbohydrates with non-starchy vegetables, like leafy greens, tomatoes, cucumbers, etc. Experiment with cooking your vegetables in different ways to find cooking styles you enjoy! Boiling, sautéing, grilling or enjoying raw over salads are diverse ways to enjoy vegetables.
- Do not exceed 2-3 servings of fruit a day. Enjoy 1-3 small dates or 1 large medjool date to break your fast as 1 serving. Try to break your fruit servings between your suhoor and 2 iftar mini-meals. Balance your intake of fruits with other food groups, for example, yogurt or cottage cheese to increase protein content and make you feel fuller longer.
For more healthy meal ideas and iftar and suhoor guidelines, download our FREE Healthy Ramadan Checklist HERE.
Diabetes Management After Ramadan
Once Ramadan concludes, patients with diabetes must be extra vigilant to ensure a smooth transition into regular non-fasting diabetes management. This involves paying special attention to food choices and medication doses in the days immediately following Ramadan:
It is important that physicians should advise individuals with diabetes about the risk of developing hyperglycemia after Ramadan. Ramadan is followed by a 3-day festival known as Eid al-Fitr. This festival is usually celebrated with sweets and gifts and the potential for high calorific intake. It is, therefore, important that physicians should also emphasize the importance of resuming medications as normal and not in reduced doses. (6)
Speak with your doctor to formulate an individualised plan for before, during and after Ramadan to best manage your diabetes!
Remember, it is your RESPONSIBILITY to your body to ensure you are creating a safe condition for fasting. Your body’s chronic condition needs to be respected:
The Prophet ﷺ said: Verily, your body has a right over you.
If you are not advised to fast by your medical doctor, please, take this recommendation seriously. If you are permitted to fast, ensure that you are maintaining the steps outlined in this article to have a safe and enjoyable Ramadan inshAllah!
Healthy FOOD, EXERCISE and SLEEP must come together for your HEALTHIEST Ramadan ever! Luckily, we’ve got you covered!
The Ramadan Reset eBook is your complete solution to healthy eating, exercise, sleep, coffee and so much more in Ramadan! With 90 dietitian-created recipes, full fasting fitness schedules for ALL levels, your Ramadan will never be the same! Click HERE to learn more!
Recommended Reading:
ARTICLE: Hypoglycemia (Low Blood Glucose) by the American Diabetes Association
ARTICLE: Hyperglycemia (High Blood Glucose) by the American Diabetes Association
ARTICLE: Diabetes and Fasting During Ramadan by the Hamad Medical Corporation
BOOK: The Diabetes Code: Prevent and Reverse Type 2 Diabetes Naturally by Dr. Jason Fung
References
- Mojaddidi, M., Hassanein, M., & Malik, R. A. (2006). Ramadan and diabetes: evidence‐based guidelines. Prescriber, 17(17), 38-43.
- Salti, I., Bénard, E., Detournay, B., Bianchi-Biscay, M., Le Brigand, C., Voinet, C., & Jabbar, A. (2004). A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes care, 27(10), 2306-2311.
- Hassanein, M., Bravis, V., Hui, E., & Devendra, D. (2009). Ramadan-focused education and awareness in type 2 diabetes. Diabetologia, 52(2), 367.
- Zabeen, B., Tayyeb, S., Benarjee, B., Baki, A., Nahar, J., Mohsin, F., … & Azad, K. (2014). Fasting during Ramadan in adolescents with diabetes. Indian journal of endocrinology and metabolism, 18(1), 44.
- Hassanein, M. (2015). Ramadan focused diabetes education; a much needed approach. J Pak Med Assoc, 65(5 Suppl 1), S76-S78.
- Ahmed, M. H., Husain, N. E., Elmadhoun, W. M., Noor, S. K., Khalil, A. A., & Almobarak, A. O. (2017). Diabetes and Ramadan: A concise and practical update. Journal of family medicine and primary care, 6(1), 11.
- Benaji, B., Mounib, N., Roky, R., Aadil, N., Houti, I. E., Moussamih, S., … & El Ghomari, H. (2006). Diabetes and Ramadan: review of the literature. Diabetes research and clinical practice, 73(2), 117-125.
- Hui, E., Bravis, V., Hassanein, M., Hanif, W., Malik, R., Chowdhury, T. A., … & Devendra, D. (2010). Management of people with diabetes wanting to fast during Ramadan. Bmj, 340(22), 3053-3053.